We’d like to invite you to Palliative Pupus our exciting local networking and clinical education opportunity. Come participate in an interactive interdisciplinary story from the cutting edge of hospice and palliative care and mingle with colleagues.
If you are involved with palliative care cases, you are invited. Please tell your colleagues and friends.
Please join us on from 5:15 PM – 7:00 pm at Queen’s Conference Center for Palliative Pupus.
- Palliative Pupus meets in Room 200 on the second floor of the Queen’s Conference Center
- Topic is announced in a Kōkua Mau reminder eNewsletter one week prior to the event
- Bi-monthly: every third Wednesday of the month
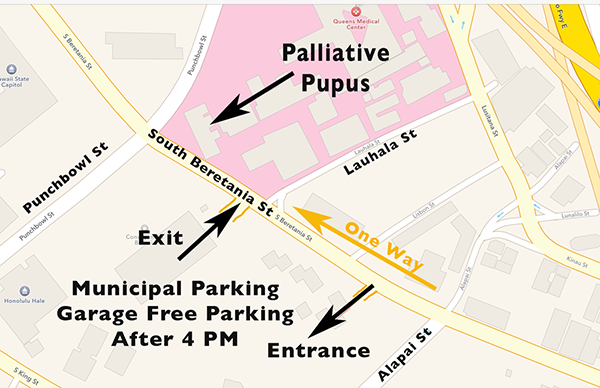
The Queens Conference Center (QCC)
Room 200
510 S. Beretania Street
Honolulu, HI 96813
Palliative Pupus 2017 dates:
March 15 • May 17 • July 19 • September 20 • November 15
- More on parking near QCC
How does Palliative Pupus work?
The theme and presenters for each ‘Palliative Pupus’ is announced one to two weeks prior to the meeting date via our Kokua Mau eNewsletter. If you are not receiving our eNewsletter yet, please subscribe here and we will keep you informed.
Please RSVP as soon as possible to Jeannette Koijane. There is validated parking for the first 15 people who request it with their RSVP. Others can feed the meter machine across the street at the DOH (which now has a two hour maximum enforced 24 hours, according to the new sign).
What is Palliative Pupus?
Our first successful Palliative Pupus meeting was held November 17, 2010 and has since become a bi-monthly event every third Wednesday of the month. (Except November due to Thanksgiving)
- Palliative Pupus is a potluck event so please bring food to share.

Please note:
There is FREE parking after 4 PM in the municipal lot on South Beretania, just Diamond Head of Queen’s. You may have to look a bit, but free is hard to beat downtown.
Examples of Palliative Pupus themes:
Wed. July 2017
We heard one care team’s journey responding to a request for futile care from a dying patient.
Wed. Dec. 2, 2015
This month we will hear about a man’s spiritual and existential distress and the ways the palliative care providers facilitated his and his family’s coming to terms with his last weeks of life.
Wed. 9/16 2015
This month’s case features a patient, family, and interdisciplinary team supporting each other when a 21 year-old presents with incurable disease.
January 15, 2014:
Please join us for another dynamic, inter-disciplinary, case-based discussion from the cutting edge of hospice and palliative care. This month, a man with end-stage heart failure is “stuck” in intensive care unless a sophisticated individualized hospice care plan can be developed. Learn about new ways to care for people with advanced heart failure and their families in Hawaii.
July 17, 2013 theme: In this session, using our case-based format, we hear how the palliative care program at Kaiser has learned to turn withdrawal of life support into a family-centered ceremony of remembrance. Please feel free to bring a friend and perhaps a pupu to share.
May 15, 2013 theme: This month will feature cases from the cutting edge of hospice and palliative care. We will hear about successful upstreaming of access to hospice and palliative care in the Queen’s Medical Center emergency department.
March 20, 2013: This March meeting will feature discussion of a pediatric hospice patient, born with a terminal neuromuscular illness. The child’s parents will join the hospice team in discussing their journey.
January 16, 2013: This month’s case will feature transitions in care for a patient between outpatient palliative care, acute care, and hospice. Other themes for discussion will include management of problem opioid-taking behaviors in hospice and challenges to care posed by non-adherence to medical care.
July 18, 2012: This month’s case discussion will again follow a patient from diagnosis, through disease-directed treatment, hospice care and death. Features of the case that will be discussed will include caring for young adults, caring for patients with a history of mental illness and chemical dependence, timely transition to hospice, and palliative sedation in the home.
May 16, 2012: This month’s discussion will feature a case where the hospital-based palliative care team and the home hospice team had to resolve mutual concerns for patient safety including the potential for domestic violence. In a broader sense we will consider: when is it not safe to go home and who decides?